The Challenges of Building a Remote Patient Monitoring System
Nonadherence leads to 25% of hospitalizations
The primary objective of healthcare companies is to provide effective treatment, which includes proper diagnosis and timely care. It is also crucial to ensure that patients follow medical prescriptions. Affecting the length and quality of life, medical adherence has a direct impact on health outcomes. However, people often fail to comply with doctor instructions, which results in health deterioration and economic burden.
In the US, nonadherence can account for up to 50% of treatment failures, with nearly 125,000 deaths and up to 25% of hospitalizations annually. Although optimal therapeutic efficacy requires an adherence rate to chronic medications of at least 80%, it generally ranges between 50%–60%.
The World Health Organization (WHO) reports that in developed countries, such as the US, only 51% of patients with hypertension adhere to the prescribed course of treatment. In Australia, just 43% of people with asthma take medicines according to doctor instructions.
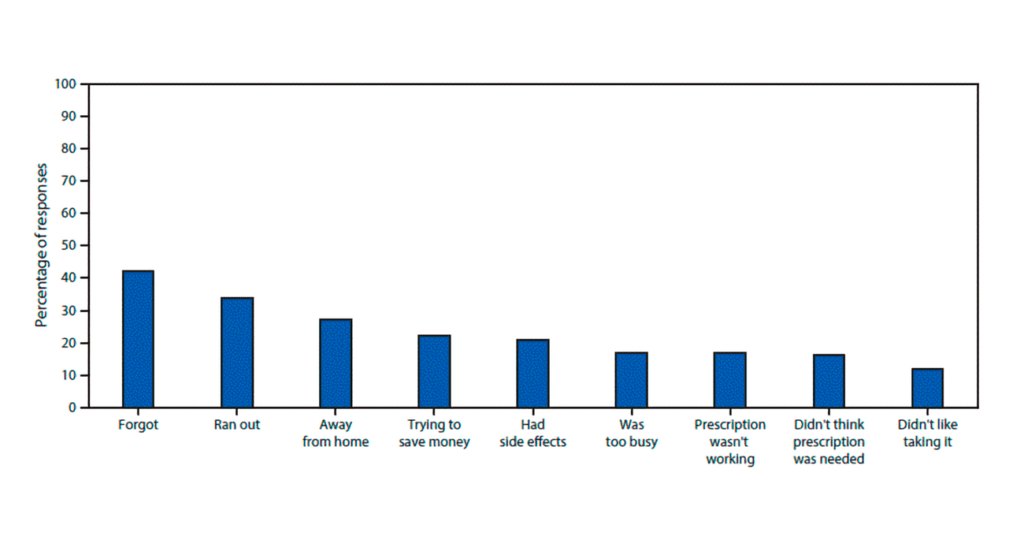 Reasons for nonadherence to medication regimens (image credit: CDC)
Reasons for nonadherence to medication regimens (image credit: CDC)Analysts at the WHO also found out that adherence to medication among elderly patients with moderate-to-severe asthma resulted in a 20% decrease in annual hospitalizations. At the same time, potential savings from optimal treatment control of severe asthma could potentially account for 45% of healthcare costs.
The Centers for Disease Control and Prevention (CDC) informs that the total healthcare costs associated with nonadherence in the US have grown to $100–$300 billion per year already.
Alongside nonadherence, medical organizations encounter other challenges. For instance, the elderly and people with varying types of physical disabilities often are not able to visit clinicians in person. Furthermore, it may be impossible to provide timely assistance and enough space in hospitals during disruptions such as the coronavirus pandemic.
The COVID-19 pandemic has dramatically changed the way people use traditional healthcare. According to a national survey conducted by the Alliance of Community Health Plans (ACHP) and the Academy of Managed Care Pharmacy (AMCP), 41% of US customers postponed healthcare services, 42% of respondents said they felt uncomfortable going to a hospital, and 38% planned to delay future treatment due to coronavirus. Though 58% of participants considered their doctors as the most trusted source of information on the COVID-19 disease, only 31% felt comfortable during in-person visits.
As a result, telehealth has witnessed considerable growth. ACHP estimates that its usage nearly tripled in 2020 compared to 2019. According to the organization, 28% of patients used some form of telehealth at the beginning of 2020, and 89% out of them were satisfied with the experience.
Remote patient monitoring (RPM) powered by the Internet of Things (IoT) technologies can address the issues described above—at least, partly. By capturing real-time patient data (e.g., heart rate, blood glucose level, oxygen level, arterial pressure, etc.) and sending it to the system used by healthcare providers, RPM systems can track medication adherence, identifying potential risks and managing prescriptions.
This way, medical institutions can improve the quality of care and increase overall efficiency during the pandemic. Still, huge amounts of telemetry data—as well as regulations, privacy, and integration issues—make this initiative not an easy task.
This article describes what medical organizations need to know when enabling remote patient monitoring, as well as how to address the technical challenges when building such a system.
The components of an RPM system
To ensure patient health monitoring (RHM) outside clinics, medical institutions and individuals need to employ IoT equipment, such as connected devices and sensors (e.g., wearables). The rise of the IoT in healthcare has led to the growing adoption of glucose meters, smart inhalers, heart rate monitors, and other similar tools.
Collecting patient data, devices and sensors send it to a cloud-based system for further analysis by healthcare professionals. While clinicians utilize dashboards for data visualization and prescription management, patients commonly rely on mobile apps to share data and communicate with doctors. A mobile app can also remind users to take medicines, promoting adherence.
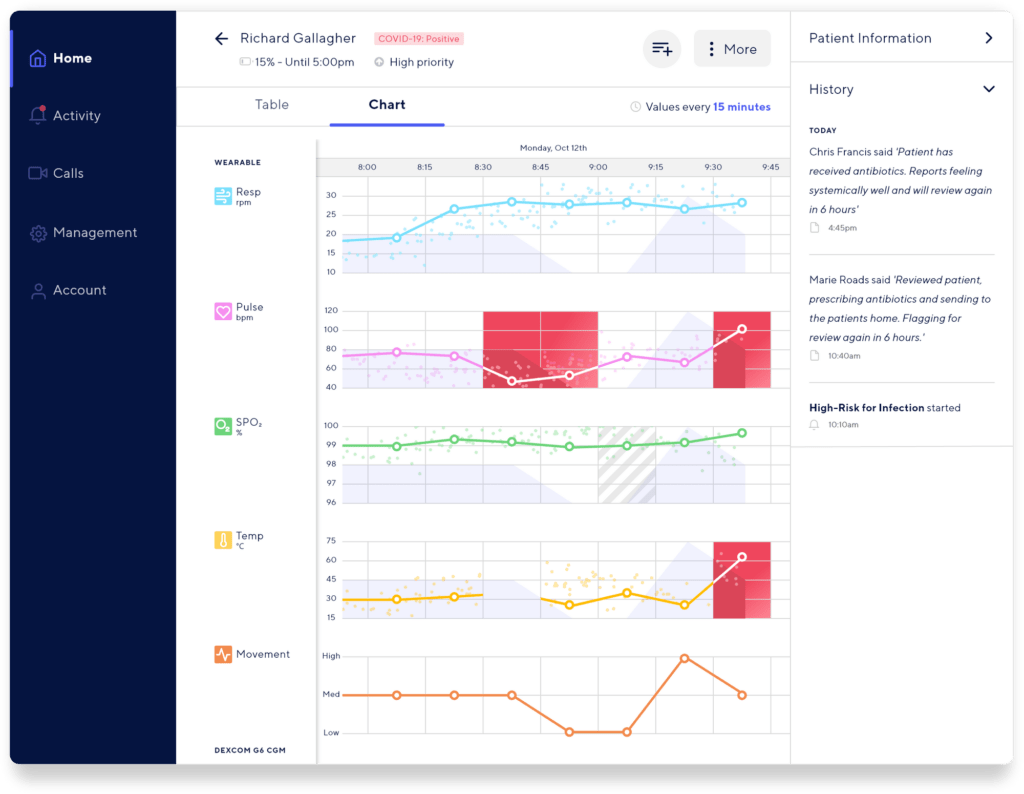 An example of a patient data dashboard (image credit: Oracle)
An example of a patient data dashboard (image credit: Oracle)Therefore, a remote patient monitoring system may consist of the following modules—from a high-level perspective:
- Data collection. Medical organizations can use sensors and smart devices to measure a variety of health indicators (for instance, an electrocardiogram, arterial pressure, or a peak expiratory flow rate). Collected “on the edge,” data is then sent to a web system for storage and analysis.
- Cloud storage. To record massive—and ever-changing—arrays of data, a remote patient monitoring system has to employ a scalable data storage capable of handling thousands or even millions of requests per second.
- Data processing. A software platform has to aggregate data from multiple sources and process it to gain a real-time view of health condition, as well as instantly alert doctors and patients about potential issues. This way, clinicians will be able to monitor various health indicators (e.g., a heart rate and/or blood glucose level), as well as identify and assess risks.
- Dashboards. Healthcare institutions can implement dashboards to enable doctors to monitor treatment regimens, manage prescriptions, analyze electronic health records (EHR), and visualize patient information in real time. It is also important to provide access to the history of treatment and communication with patients.
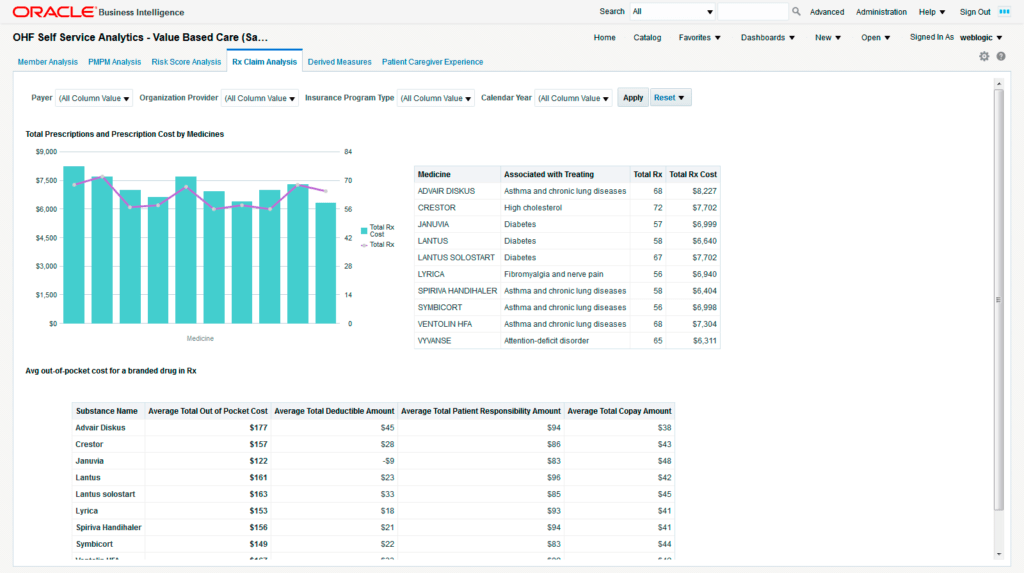 An example of online prescription management (image credit: Oracle)
An example of online prescription management (image credit: Oracle)- Communication engines. With these, doctors and patients are able to share data and medical prescriptions. Healthcare experts have to be instantly alerted about health deterioration, while a remote health monitoring app can remind patients to take medicines.
- An administration panel. Employing this module, healthcare institutions can add new patients and clinicians to the system, manage user roles and permissions, etc.
Depending on specific needs, other components (e.g., video conferencing, a location assistant, or appointment scheduling) may be included in a remote health monitoring system or be implemented as part of the modules described above.
To deliver a software platform containing these modules, one can utilize a scalable cloud architecture, such as Amazon Web Services (AWS) or Microsoft Azure.
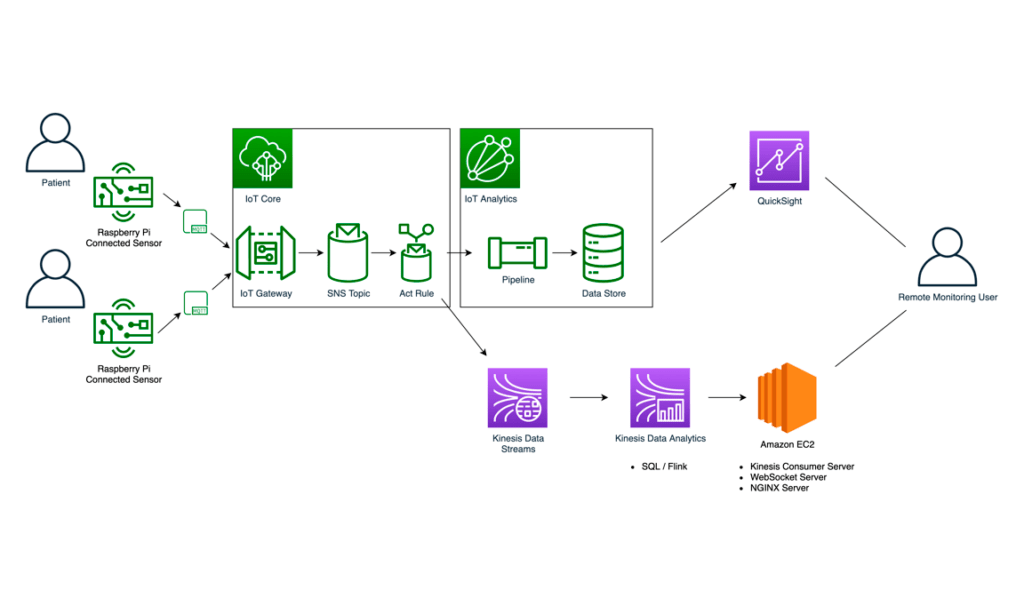
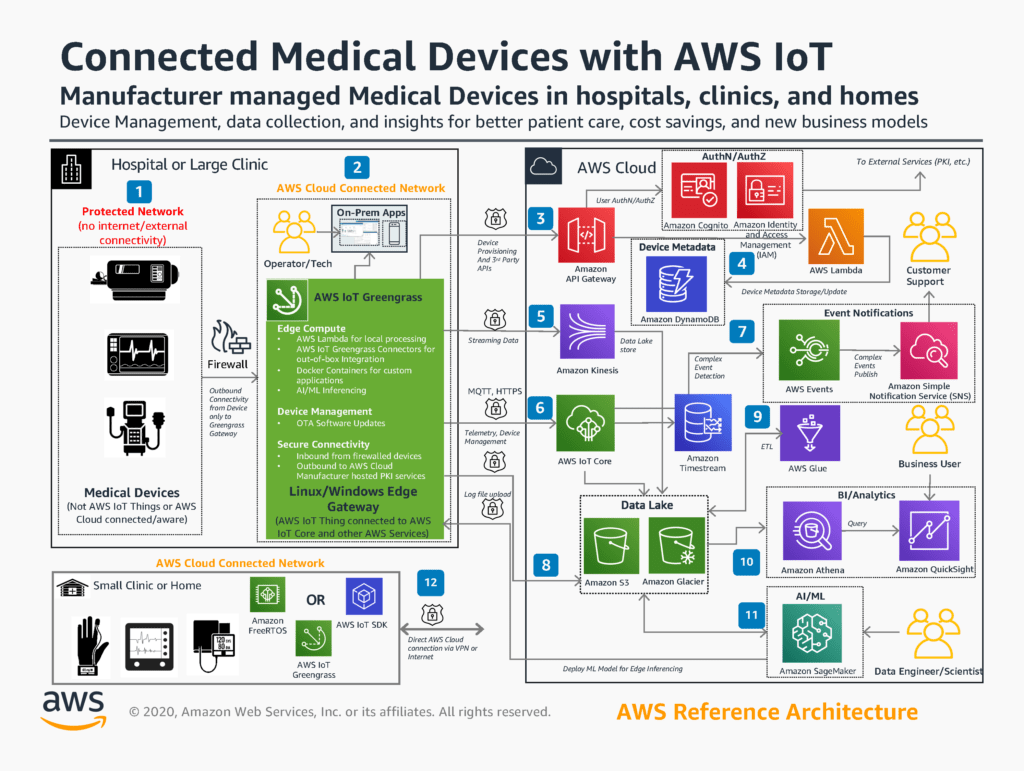 A reference architecture of a remote patient monitoring system (image credit: Amazon)
A reference architecture of a remote patient monitoring system (image credit: Amazon)Using the reference architecture above as an example, Amazon describes what is needed to enable data storage, predictive analytics, notifications, etc., as well as how to connect various components using APIs. Depending on your treatment delivery process, the workflows may differ.
(This documentation from Microsoft serves a very similar purpose.)
Four challenges around building an RPM system
When developing a system for remote health monitoring, engineering teams may face the following issues.
1. Storing and processing massive arrays of data
A remote patient monitoring solution collects health data from sensors and smart devices, which number may range from hundreds to millions. In this regard, the platform has to capture and write terabytes of data per second. While data volume generated by hardware increases, so do response times. As a result, it becomes hard to process data in real time. Therefore, a remote health monitoring system has to collect, transfer, save, and analyze patient data without an adverse effect on performance.
To ensure the platform can store and ingest terabytes of information per second, a healthcare organization may opt for NoSQL data stores that can scale out by utilizing commodity hardware instead of adding more servers. Systems such as Couchbase, MongoDB, or Cassandra can sustain heavy traffic, while providing better performance compared to SQL-based relational databases.
Building a data lake is also a good idea to store and process raw, structured, and unstructured data collected from IoT devices and mobile apps in a centralized and unified manner. Data lakes are of a great help when it comes to further data transformations: analysis, visualization, reporting, etc. To process data in a data lake, you may use a bunch of mature tools, such as Apache Spark, Hadoop, Hive, etc.
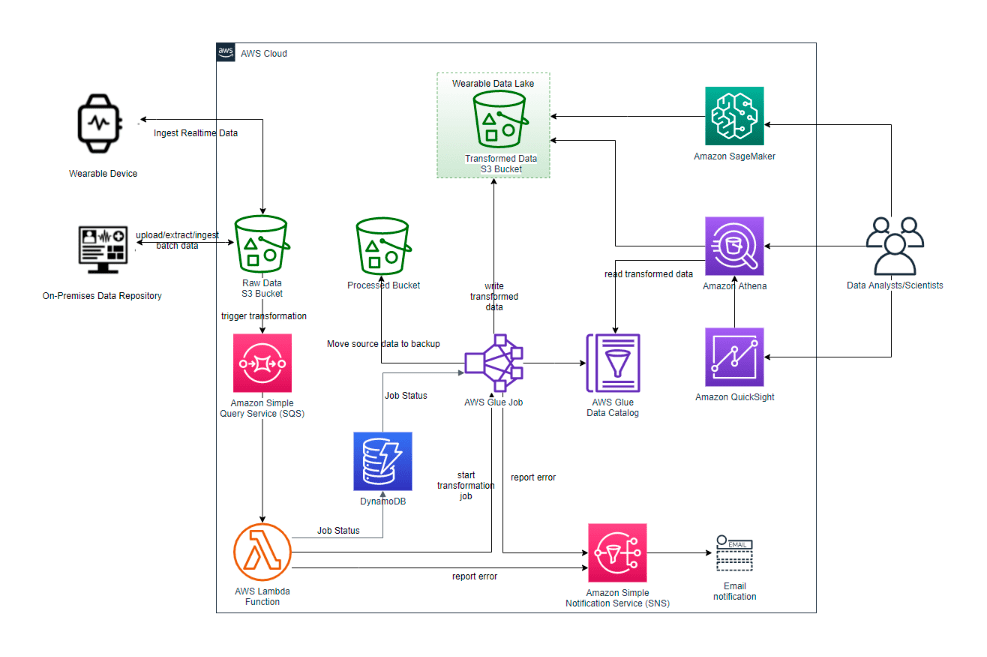 A possible data lake architecture (image credit: Amazon)
A possible data lake architecture (image credit: Amazon)
2. Scalability and high availability
An RPM solution has to process data in real time to identify and prevent potential health issues as they appear. This way, the availability of the platform is crucial to delivering treatment without delays—otherwise, patient lives are at stake. In this regard, it is also important to sustain a continuously growing number of user requests. For this purpose, on-demand scaling has to be enabled, as well as stable, uninterrupted performance.
Consider building a microservices-based system represented by loosely coupled components that can be developed, deployed, and maintained independently from each other. Unlike monoliths, microservices give you room to utilize different technologies (programming languages, frameworks, libraries, etc.), as well as expand and maintain the components without refactoring the whole system.
Organizations can enable load balancing and autoscaling of computing resources, so that a remote patient monitoring system scales up or down depending on the load. Additionally, medical institutions can automatically replicate data across multiple availability zones, cloud resources, and data centers, this way reducing latency regardless of user location. Platforms such as Kubernetes can help with operations automation.
To reduce latencies and improve privacy, one may rely on edge computing, a distributed computing paradigm that brings computation and storage closer to sensors and connected devices. Thanks to this, healthcare facilities can minimize bandwidth and response times—and, therefore, prevent delays in treatment.
 A sample module collecting patient data on the edge (image credit: Amazon)
A sample module collecting patient data on the edge (image credit: Amazon)
3. Security and compliance
Since remote patient monitoring systems store and process sensitive data—electronic health records, diagnostic results, etc.—proper security and privacy have to be ensured. Healthcare is a highly regulated industry, so it is crucial to achieve compliance with all the required standards, such as HIPAA and HITECH in the US, as well as GDPR in the EU.
It is worth noting that users of wearables are highly concerned about the confidentiality of data they share. According to Deloitte, among those Americans who employ fitness trackers and smartwatches to monitor physical activities, heart rate, possible COVID-19 symptoms, etc., 40% are concerned about the privacy of the information collected by their devices. Deloitte also reports that these concerns significantly increase—up to 60%—among those users who subscribe to reports based on their health and fitness data.
To ensure security and compliance, healthcare providers have to implement features such as two-factor authentication, role-based access control, data encryption, etc. It is also important to instantly detect suspicious activities, assess risks, and prevent threats with full-stack infrastructure monitoring.
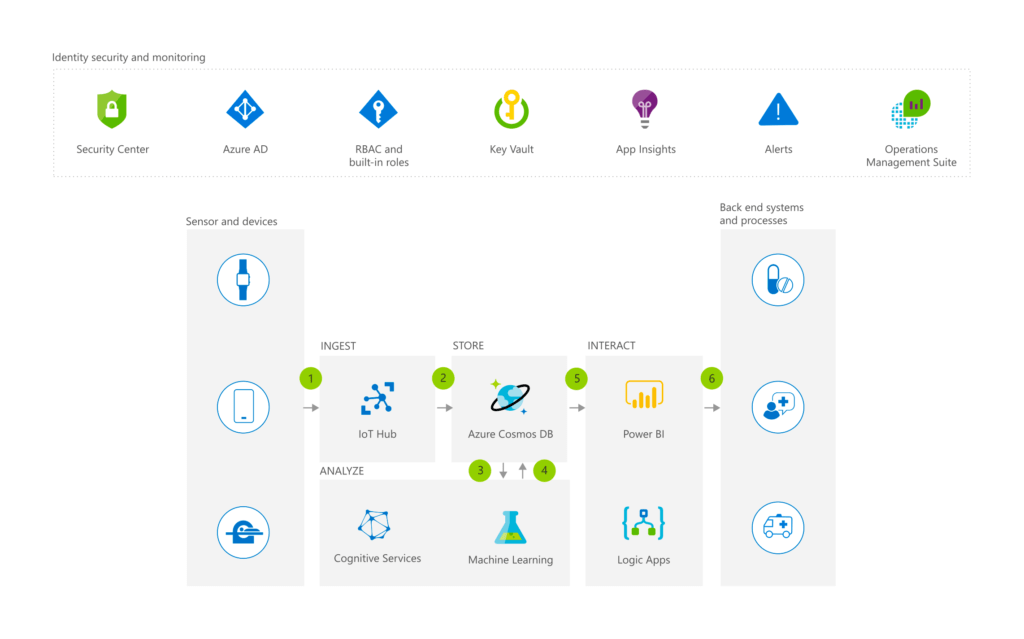 A secure remote health monitoring architecture based on Azure (image credit: Microsoft)
A secure remote health monitoring architecture based on Azure (image credit: Microsoft)
4. Integration
The patient data aggregated from various sources can be obtained in numerous formats, including unstructured or semistructured ones. Furthermore, there are different manufacturers of wearables and sensors that do not use a common data standard. Besides, a remote health monitoring solution has to be integrated into a software ecosystem that already exists within a given organization.
To provide a unified view of health data (i.e., procedures, medical prescriptions, diagnoses), a healthcare company can build a single data repository for telemetry from sensors, smart devices, and apps. When connecting hardware with software, a medical institution can then rely on data lake patterns for extracting, transforming, and loading (ETL) patient information. By introducing data quality initiatives, it is possible to prevent the transfer of outdated or duplicated information between the integrated systems.
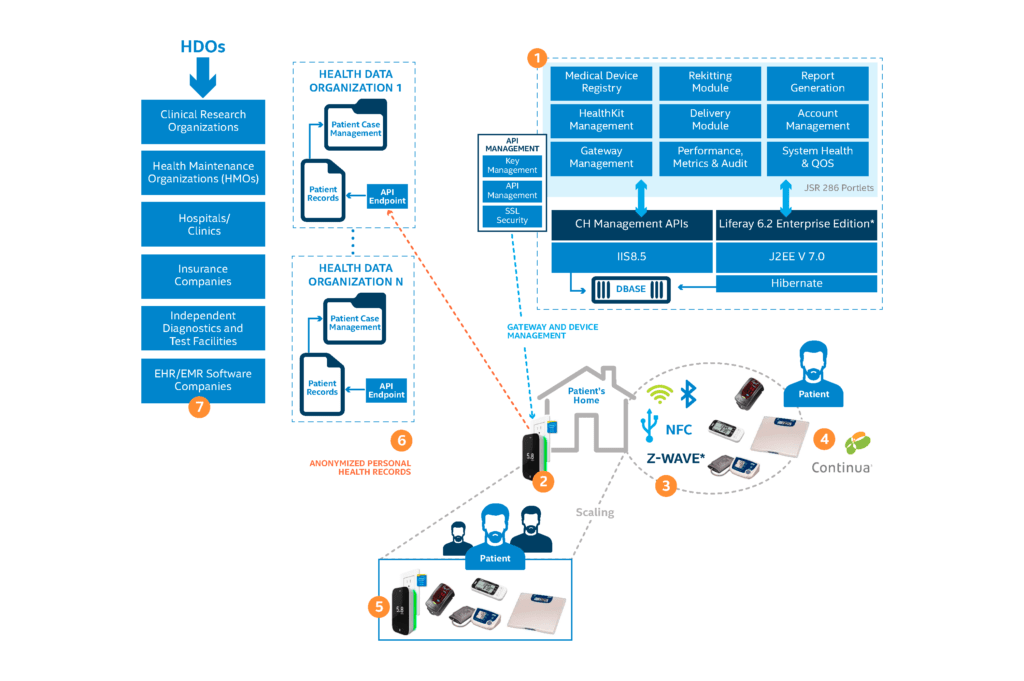 An integrated architecture of a remote patient monitoring system (image credit: Intel)
An integrated architecture of a remote patient monitoring system (image credit: Intel)It is also important to ensure compliance with the Fast Healthcare Interoperability Resources (FHIR) standard, which promotes the use of application programming interfaces (APIs) to provide EHR interoperability and improve health data unification. When integrating healthcare systems via APIs, caregivers must pay attention to securing networking protocols and can also automate API management.
The use of virtual care grows
The growing adoption of remote patient monitoring systems is being fueled by the increasing need to facilitate access to healthcare services, provide timely assistance, and increase efficiency. Analysts at Deloitte revealed that, even before the COVID-19 pandemic, the use of virtual health care was gradually increasing. For instance, the number of video visits surged from 14% to 19% between 2018 and 2020, while the usage of remote health monitoring at home doubled, growing from 6% to 13%. Remote care management and coaching also saw significant growth, rising from 8% to 14%. In 2020, physician-to-physician consultations grew from 17% to 22%. While 14% of doctors conducted online visits in 2018, already 19% reported doing so in early 2020.
For primary care physicians, remote care management rose from 11% in 2018 to 21% at the beginning of 2020. The proportion of clinicians communicating with patients through electronic health records saw a considerable increase from 38% in 2018 versus 63% in early 2020.
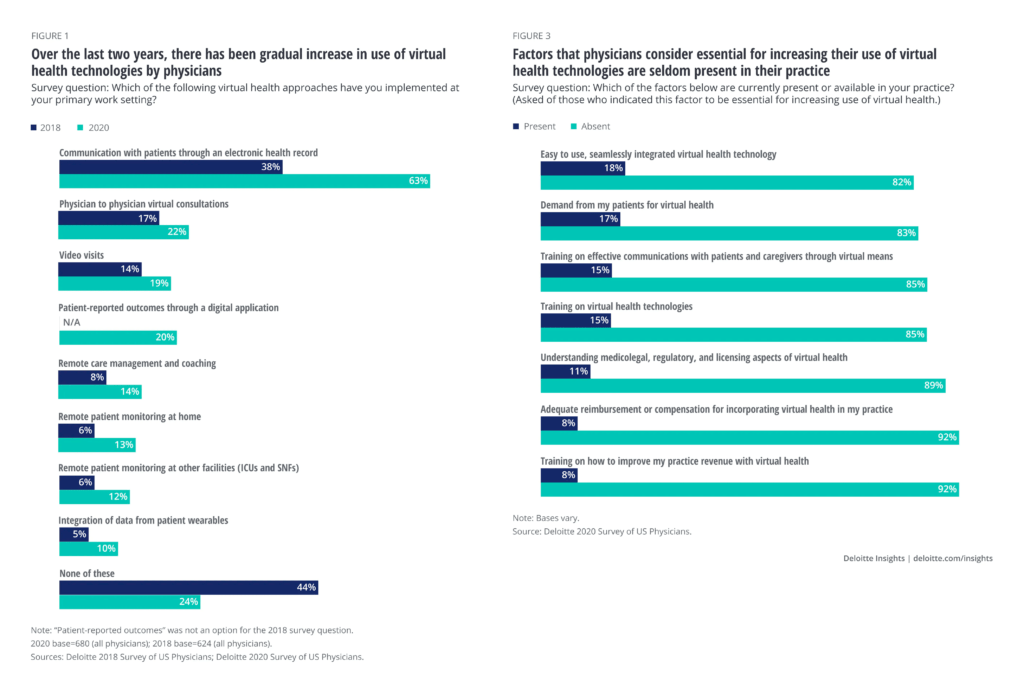 An increase in virtual care adoption and concerns raised (image credit: Deloitte)
An increase in virtual care adoption and concerns raised (image credit: Deloitte)Obviously, these numbers have grown further since the pandemic started. In 2020, a study by McKinsey discovered that “health systems, primary care, and behavioral health practices are reporting increases of more than 50x–175x in telehealth visits.”
McKinsey also projected an overwhelming potential of virtual care to generate revenue by 2022. Estimated to accumulate 113% under the compound annual growth rate, virtual care significantly outperforms other in- and outpatient options all together. So, currently, this healthcare area can provide a decent return on investment (ROI) helping to minimize the losses introduced by the pandemic.
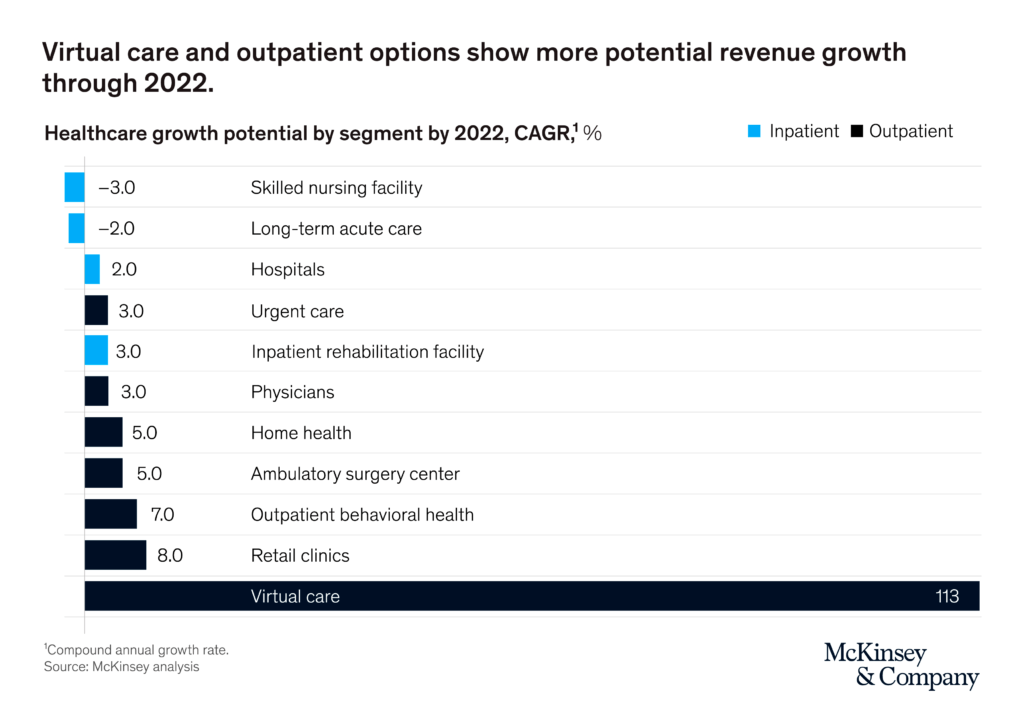 The potential of in- and outpatient options to drive revenue (image credit: McKinsey)
The potential of in- and outpatient options to drive revenue (image credit: McKinsey)However, there are some barriers to the adoption of remote patient monitoring software and virtual care, of course. Deloitte informed that, prior to the pandemic, nearly 89% of physicians reported the lack of critical elements, such as clarity around regulatory, licensing, and medicolegal aspects. In addition, 85% of doctors complained about the absence of proper training around the means of establishing effective virtual communication with patients.
To enable remote patient monitoring, medical organizations have to invest in IT infrastructure to collect, store, and process health data, while ensuring smooth interaction between doctors and patients via telemedicine apps. Healthcare facilities may also need to adapt their workflows to new models of delivering treatment, provide remote care training, consider licensing, and address arising issues.
However, if implemented properly, remote health monitoring may considerably improve diagnostics and treatment, as well as boost the productivity of clinicians, allowing them to review more requests and emergency cases per day.
To learn more about improving patient treatment with telemedicine and health information technology, download our research paper on the topic.
Further reading
- The Pitfalls of Creating Appointment Scheduling Apps for Healthcare
- The Technical Side of Embedding Video Calls into Telehealth Apps
- 15 Ways Telemedicine and Health Information Technology Can Improve Patient Care